How wound healing works in diabetics
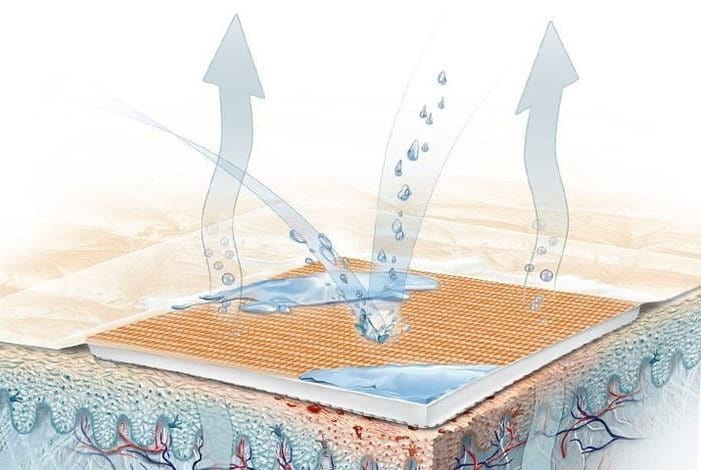
Our skin acts as a barrier between outside germs and bacteria. When an abrasion forms on the skin, the barrier is broken and the wound is left exposed. If harmful bacteria enters the wound at this stage, it has the potential to cause an infection and further complications. In healthy bodies, white blood cells rush to the wound site to destroy bacteria and protect the body from infection. Only after this stage does the tissue regrowth stage begin and the wound gets patched up.
In diabetics, the body is unable to produce or use a hormone called insulin. Because of this, the blood sugar level increases which has adverse effects on wound healing. When blood sugar levels rise, they impair the functioning of white blood cells (WBCs). WBCs are imperative for the functioning of the immune system, and without them the body is unable to fight off infection efficiently.
If diabetes is not kept under control, it affects blood circulation as well. Slower blood circulation hampers the healing process of the wound as the nutrient supply to the wound site slows down. Oxygenation of the wound site is also vital in the healing process, and slower blood circulation means slower oxygenation. Another risk factor is that diabetes can cause neuropathy (nerve damage) which is the numbing of sensation in parts of the body. Due to this, the diabetic patient might not realize that they have sustained an injury as they will not feel it.
Common diabetic wounds:
General tips to follow if you are a diabetic:
Factoring in the increased risk of infection, diabetic patients need to be very careful while caring for their wounds. As they say, prevention is better than cure. Remember to:
- Always wear comfortable footwear
- Do not pick or itch at scabs or dry skin
- Make sure to moisturize so that your skin stays strong and doesn’t flake
- Be careful not to snip your skin when you’re trimming your toenails
- Wash and inspect your feet daily
- Stay on top of your blood sugar levels and ensure optimum diabetic care
A wound care checklist for diabetics:
Wounds are inevitable but we should do all we can to prevent them when possible. If you have sustained a cut in any part of your body, follow the appropriate wound care procedure immediately. Here are the steps to follow to properly clean and care for a diabetic wound:
- Clean the wound with saline solution or warm water to clear out skin debris and dirt
- Apply an antibiotic ointment for faster healing time
- Wrap a clean gauze pad around the wound or use a plaster
- Follow your diabetes treatment regime strictly and keep a check on your blood sugar levels to ensure there’s no alarming rise
- Don’t put unnecessary pressure on the wound
Keeping all of these factors in mind can help you to correctly treat your diabetic wounds and ulcers and stay free from infection. Read More Here: How To Treat a Foot Corn Effectively